How I Almost Died
Back in 2014, I almost died. Here's my story.
How do you start to tell someone that you nearly died? That your wife watched you in intensive care, fighting for your life? That your children nearly lost their father when he was only 42?
It's a story I never thought I'd have to tell but I've spent the past couple of years recounting this tale to many people. They're interested yet shocked. They want to know more yet almost always squirm at the details. Most people can't believe it happened. I often can't believe it happened. It feels like a really bad dream or a fly-on-the-wall documentary. I've wanted to write it down since it happened but never felt able to do it. So finally here it is: a brief account of how I almost died.
The beginning
June 2014 started of as a normal month. My son's 7th birthday in early June. My best mate Mark's annual birthday party in the middle of the month which always involves a few beers and DJing some tunes to celebrate, this year being his 43rd birthday. On Wednesday 18th June, a train ride down to the BBC offices in London to talk about our team becoming part of the myBBC initiative. Post-meeting we gathered for some food at an African restaurant around the corner from Euston station. Some deliciously hot and spicy jerk chicken was devoured with some not-so-tasty, in my opinion, African ginger beer. Nothing unusual and I returned home to Warrington on the train having eaten my last solid meal in what would become a couple of months.

The illness starts
The next day is when it started. "It" was me feeling "a bit poorly", as your mum might say. I came home from work because I was feeling intermittently hot and cold. From previous experience, this was a tell-tale sign of a stomach bug and sure enough, the evening was filled with the joy that is vomiting and diarrhoea. I texted my boss to tell him I wasn't going to be in on Friday morning as I'd been up all night throwing up. I felt terrible because I had to cancel my plans to give a lesson at his wife's school where we'd planned to teach 10 and 11 year olds how to write videogames. My wife Clare thought it was unusual for me to be so sick and took me to the doctor. The doctor gave me some Dioralyte sachets to rehydrate myself with and sent me home. Over the weekend I attempted to take them and to drink lots of the classic British cure for illness, Lucozade. I couldn't keep either down. Family plans were cancelled as I continued being ill all weekend. Clare quickly ushered me to the doctor again on Monday morning, noting that I was having difficulty even walking which seemed somewhat unusual for a case of gastroenteritis. The locum doctor was at the surgery and he examined me much more closely. Apparently touching my stomach made me cry out in pain. I have no recollection of this but it was enough for him to refer me to the Accident and Emergency department immediately. The symptoms appeared more serious to him than were first imagined.
I think he was probably the first person to save my life.
Accident and emergency
This is where my memory starts to get hazy and my wife's memory takes over. She'd already taken the morning off work, having needed to drive me to the doctor's surgery, so she drove me to the Accident and Emergency department at Warrington hospital. I almost collapsed while trying to sit down in the waiting room and thankfully the doctor's referral note meant a swifter move through the triage to be seen by one of the A&E doctors. They realised that I was massively dehydrated, having not managed to keep much liquid down for nearly 5 days, and I was admitted to a ward. I was taken to a separate room rather than a ward with other patients. Understandably, you can never be too sure how contagious a patient is when you don't know what they've got. I was given intravenous (IV) fluids and left while the NHS staff looked after me and tried to determine what was wrong. Clare brought the children to visit and by Tuesday she was told that I was looking better, although she noted that I was very confused. I remember being convinced that the son of a friend of ours had been killed in a car accident. I forced her to Google it on her phone but thankfully she couldn't find anything. I'd been given morphine for the pain, which probably explains why I was having vivid hallucinations, but they still weren't sure what was wrong. Apparently I told the consultant that I was feeling fine and that he should send me home. He was wise enough to realise that another day in hospital was a good idea.
He was probably the second person to save my life.
Then it happened
Apparently, it all happened very fast. Clare left me at the hospital after visiting until 7pm having been told that I was doing well. She rang again at 10pm to check I was ok and the person who answered the phone said I was fine. She was then rudely awoken at 2.30am on Wednesday morning by the phonecall you never want from a hospital, "You need to come to the hospital immediately. Marc is very ill." My blood pressure had dropped through the floor. I had multi-organ failure and all of my major organs were beginning to shut down.
“You need to come to the hospital immediately. Marc is very ill.”
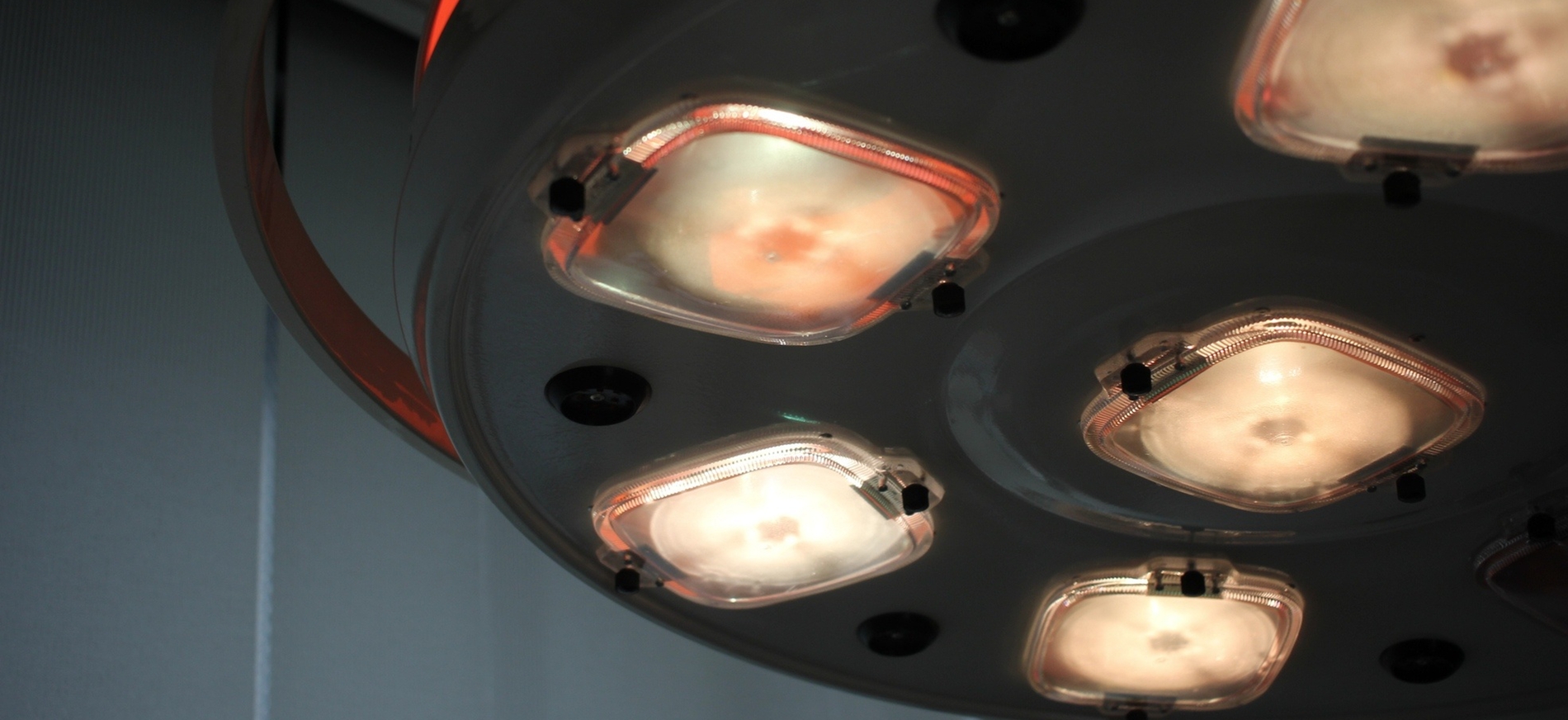
The symptoms seemed to be those of sepsis, a condition where the body's immune system goes into overdrive and attempts to protect itself from infection. I was rushed down for a computerised tomography (CT) scan to get a better picture of what was causing the drop in blood pressure. My wife had a worrying wait at 4am as the on-call CT radiologist raced to get into the hospital for this emergency procedure. The scan showed a problem somewhere in my bowel but it wasn't immediately obvious what it was. The order was given to operate that morning to investigate and potential fix the problem with my bowel. Thankfully, one of their best colorectal surgeons was on hand to perform the operation but there was no guarantee that I would survive.
Saving my life
The operation had concluded that I had an ischemic bowel due to an inadequate blood supply, but the consultants were unsure what was causing it. The infected piece of bowel was removed and an ileostomy was performed, meaning that my small bowel was diverted out of my body. This was done to attempt to allow the bowel to recover but this meant I would have a stoma, an opening in my stomach through which the waste travels into a bag. Not very glamourous but at that point in time it gave the medical staff the only chance to save my life. They took a sample from my bowel and this was sent to the microbiologists in order to find the cause of the infection. I was given broad spectrum antibiotics in order to kill it but these have the side-effects of killing good bacteria too. I was then put into a medically induced coma so that my body had a better chance of coping with the drugs that I was being given.
I was intubated to prevent asphixiation, meaning that a large tube was put into my windpipe to keep my airway clear. I was too weak to breathe so my lungs were now controlled by a ventilator. I was given inotropes to increase the strength of my heartbeat in an attempt to keep the blood flowing properly to my quickly-dying organs. My blood was passed through a dialysis machine to clean it of the toxins that were busy attacking me. My blood pressure was dangerously low. My body was dying but I was being kept alive by the miracle of modern medicine until they could determine what was wrong. Every treatment that they were given me had the potential to cause knock-on effects elsewhere. The ITU consultant spoke to Clare and my family and told them "his condition is deteriorating, despite increased support, and he is unlikely to survive."
“His condition is deteriorating, despite increased support, and he is unlikely to survive.”
They were pretty sure I would die that night.
Waking up in intensive care
After six or seven days in the induced coma, they started to decrease the amount of drugs they gave me meaning that I would drift in and out of conciousness. The combination of powerful coma-inducing drugs, incredibly strong painkillers, antibiotics and the fact that I had sepsis, which causes confusion and disorientation, meant that I literally had no idea where I was or what was going on. My dreams felt oddly lucid but were crazy and often involved things that I can only assume that I heard around the bedside. I'd dream that I was being held prisoner and my wife was being blackmailed to release me. I dreamt that I was being operated upon whilst on a boat in the Caribbean. I dreamt that I'd been in a fire in a Victorian building in London, only to be rescued and then subsequently stabbed and died. It's safe to say that my perceived reality was somewhat different to what was actually happening to me.

Thanks to Clare, I slowly began to regain some semblance of understanding as to what had happened as she explained to me that I was in intensive care. The microbiologists had finally discovered that I'd contracted the streptococcus group A bacteria, which is normally found on the skin and is generally harmless. However, if it gets into the blood stream or deeper inside the tissues or organs of the body, as it had in my bowels, then it becomes an invasive infection. This seemingly innocuous bacteria had become the source of sepsis and had caused my body to shut down. To this day, they still don't know how I contracted it, although for some time it was thought it was related to the jerk chicken I'd eaten the week earlier.
It took me quite a while to realise that I couldn't speak due to having been intubated and been put on a ventilator to help me breathe, as my lungs weren't functioning well enough to do so on their own. I found that I couldn't move any of my limbs either. It turns out that your muscle atrophies pretty quickly in hospital if you don't move. I quickly lost over 3 stone in weight and all of my muscle mass and it would take almost 2 years to get back to a reasonable weight again.
In total, I spent 45 days in intensive care and it was an incredibly difficult time. I was coming to terms with the fact I had been very ill and my body wasn't functioning very well. I had to learn to breathe on my own again, something that we just take for granted as we just start breathing as babies. Having to learn to wean myself off a ventilator and to use my incredibly weak lungs was a major challenge. The only way I could do it was to think about getting home to Clare and my two children and they gave me the impetus to do it as quickly as my body would let me. I then had to learn to eat again, as I had been tube fed for around 25-30 days. Again, this is something that you don't really remember doing as it happens when you're a baby, but I had to be spoon fed yoghurt and soup in incredibly small portions until my stomach was ready to digest food properly. This often involved me eating and then being quite violently sick a few minutes later. That quickly became soul destroying when you know you have to put on weight.
At this point I could still barely move so I was helped by the ITU nurses, dieticians, or family. They encouraged me as best they can but not being able to move or feed yourself is terribly frustrating. Although I couldn't move my own limbs, I needed to exercise to avoid continued muscle atrophy and the physiotherapists came daily to start an exercise programme. Initially this involved the use of a hoist which would be strapped around me and lift me out of the bed and into a chair. This allowed me to move into a seated position and I had to increase my sitting time from 5 minutes up to a few hours. It sounds crazy when you write it down but I could barely sit unaided for 5 to 10 minutes before I would become light headed due to having such low blood pressure. It was often incredibly painful, especially when my limbs were moved by the physio team, but the only way I was going to leave intensive care was by being able to have some movement. So again, I had to grin and bear it.
On to a normal hospital ward
After a month and a half in intensive care, I was eventually weaned off the stronger drugs and dialysis machine and became strong enough to be transferred to a normal hospital ward. It was a pretty scary experience as I was still unable to move much and I was used to the attention of a single nurse per patient that is require for patients on an intensive care ward. Being on a standard ward meant a 1-to-15 nurse to patient ratio and this was initially very hard to deal with. I was still coming to terms with trying to eat properly again and this was difficult given the lack of good hospital food. I appreciate that hospitals aren't five star restaurants, but when you're trying to recover from illness, the bland hospital food really doesn't help with improving an appetite, nor with your mental well-being.
The nurses on the standard wards were helpful but it was hard getting used to having to wait for care. I started to have daily physiotherapy visits and they helped me to get out of bed. I used to really look forward to their twice-daily visits as they were both a lovely team of people, and I knew that the only way I would be able to leave the hospital was by learning to walk again. Getting to the point of walking with a pair of crutches or walking frame, without fainting due to my low blood pressure, took just over another month by which time I'd been in hospital for a total of three months. By this time I had very little feeling in my feet, and still don't, and had necrotic tissue on my toes. This is when the tissue is dying, in my case due to the lack of blood to my feet whilst being given inotropes to keep me alive. I was told that I was likely to lose some of the tissue from my toes but they were unable to tell me how much. In passing, I was told by one of the ITU nurses that I was lucky I still had both feet as at one point in the first week there was discussion as to whether my feet should have been amputated in order to stem the toxic reaction that my body was having. I had to see the positives in this!
Once I'd proved that I could walk some steps, I had to be seen by an occupational therapist who would help me to recuperate from my incredible illness. I was taught to navigate a small flat using a walking frame and crutches. I had to make a cup of tea and learn to sit down and get back up out of a lounge chair. I eventually worked up to being able to make a bacon sandwich on my own to go with the cup of tea. An incredibly British thing to do but I was proud to have the energy to eventually be able to perform what was once such an basic task. Finally, with the ability to do basic tasks around the home, and with the energy to be able to climb up and down a small set of stairs, both the physiotherapist and occupational therapist agreed that I was able to come home. It was an amazing feeling to know that I'd be able to come home and to hug my wife and children properly, even if I couldn't really remember what home was like due to my mental state.
Coming home
On 18th September 2014, two days before my 90th day in hospital, I was allowed to return home. And then my recovery really began. Most people assume that when you return from hospital that you're healed. In most cases you probably are. You might have a few weeks of getting better but generally you're ok. In my case I really wasn't. I had a stoma bag to deal with. I still had a catheter that they had been unable to remove yet. I could barely walk without being exhausted or fainting. I had daily visits from district nurses who had to deal with the necrotic tissue on my feet, dressing it as best they could to help it to heal or fall of whilst being mindful of my constant worry that I'd have to have toes amputated. Eventually it became apparent that I'd need to have a debridement of the necrotic tissue, but given that it was deep on my right big toe, this actually meant an operation which ended up with the amputation of half of the toe. Looking at the bigger picture of still being alive, this seemed rather minor but it was still a mental challenge to accept that you will lose part of your body. I accepted medical opinion but I knew that it would have a knock on effect of changing my gait which would affect my ability to walk and increase the potential for further complications. Just over two years later I've had the toes on my right foot pinned and straightened due to ulcers forming due to my toes becoming clawed. I hope this is the final operation, but I'm pragmatic enough to understand that it might well not be.
After six weeks of being home, I managed to have the catheter removed, which is never a fun experience. After eight months I was told that I'd be able to have my stoma reversed, meaning that my lower intestine would be reattached and I'd be able to function normally again. It was a major operation but it felt like I was getting back to normal again. In May 2015, I had the operation and I was able to go to the toilet as I used to.
The new normal
As I write this, it is November 2016 and it is just over two years since the madness of this part of my life occurred. People often assume that I'm now better. I guess I am to a certain extent, I'm definitely better than I was when I contracted streptococcus group A and sepsis. However, I'm acutely aware that I'll probably never be fully better so we've had to define what we call the "new normal". This means that I'll probably never run that half marathon that I was training for when I got ill back in June 2014. Not being able to feel my feet properly due to peripheral neuropathy means that it will be easy for me get sores without realising it. Doing so could easily mean gettting an infection and losing more toes which is something I'm hoping to avoid in the future. Suffering from constant hypersensitivity due to the neuropathy means pretty constant pain in my feet but this is something I just deal with without much complaint. As I mentioned earlier, I'm still pretty happy that my feet weren't removed in intensive care. I've always been pretty positive about these things.
The new normal means thinking about things differently. It means planning holidays which are easy for me to deal with, where I don't have to do too much walking. It means accepting that I'll never run again but instead thinking of another way of exercising which has lower impact, such as cycling. It means setting myself new challenges and spending time with my family in the ways that I can. I'll never be the same as I was but that doesn't really matter any more. What really matters is that I'm still here with Clare and my children.
“I'll never be the same as I was but that doesn't really matter any more. What really matters is that I'm still here with Clare and my children.”
Thanks for reading this somewhat abridged version of my story. If you're interested in reading more then please take a look at Clare's blog where she writes about it in more detail and much better than I ever could. You can read our story from the beginning here. You can also consider donating to the Sepsis Trust who are helping to raise awareness of sepsis, of which there are over 44,000 deaths per year.